Healthcare Automation: Almost Everything You Need to Know

Keeping Healthcare Human with Healthcare Automation
The healthcare sector has faced many challenges over the past few years. Even before the pandemic, healthcare providers were dealing with growing problems such as aging populations and staff shortages.
The arrival of COVID-19 only magnified these issues. As staff burnout and turnover have reached record highs, waiting lists for procedures have increased. And at the same time, healthcare organizations have had to deal with greater budgetary pressures.
On top of that, healthcare organizations are continuing to transform how they treat customers. Moving from traditional approaches to integrated and personalized services. Whether that's new tailored medicines, e-commerce style services or automated processes for onboarding clinical staff.
Intelligent automation is one of the best ways for healthcare organizations to bridge gaps and drive transformation.
Did you know?The average turnover rate for healthcare staff in the U.S. grew from 17.8% in 2019 to 19.5% in 2020.
Source: Statista
How Healthcare Automation Addresses the Challenges
Healthcare automation is transforming organizations. Here are five areas where automation can have the most impact on your business operations:
- Healthcare operations and the back office
- Patient experience
- Patient outcomes
- Staff satisfaction
- Cost management
One way it improves these areas is data processing. Healthcare automation efficiently transfers data and connects systems, resulting in a single source of truth. Healthcare professionals can then easily access this accurate data and give a better patient experience.
The pandemic sped up the introduction of healthcare RPA, as to staff started to work remotely to reduce the number of Covid-19 patients. Therefore, more healthcare processes needed to be completed online. It also highlighted how automation can deliver improved healthcare services – from rapid test results to remote consultations.
Read our blog to learn how RPA helped support Singapore's Healthcare Industry
What is Healthcare Automation
Healthcare automation is the use of ‘bots’ or digital workers to improve the flow of information between people and systems. By using RPA with other technologies such as OCR and machine learning, it can source, extract, and enter relevant data. This results in removing the need to rekey data, as well as improving efficiency, patient outcomes and the experience of staff.
How Does Automation Help Healthcare
Teams within the healthcare industry often operate in silos. Each of these departments from x-ray to consultants has multiple healthcare systems they work on. And the people in these teams act as the links that move data from one system to another.
Healthcare automation replaces these human interactions with digital workers that can operate 24/7, with zero errors and at much faster speed. Not only does this help provide a better service to patients and improve staff experience, but it also helps reduce errors in back office processing.
Above all, healthcare automation releases doctors, nurses, consultants and staff to focus on patient care, rather than completing administrative tasks
What are the Benefits of Healthcare Automation

The benefits of automation in healthcare are:
- Improving healthcare operational efficiency
- Managing the cost of care
- Improve Infrastructure and Interoperability
- Boosting staff satisfaction
- Improving patient outcomes
- Enhancing patient experience
Healthcare automation provides benefits for the organization and people. Below, we’ll look at each of these in more detail.
How Does Healthcare Automation Help Organizations?
Improving healthcare operations
Although healthcare is a unique sector, many of its back-office systems are no different from other organizations. For example, automating your supply chain or inventory management processes can deliver benefits in cost efficiencies and savings.
Managing the cost of care
The inefficiencies of current siloed operations mean that it’s difficult to reduce the cost of care. Today, some providers are using digital workers to improve processes. One example is revenue cycle management (RCM), which can include as many as 20 different activities. Healthcare providers can automate most RCM activities from patient scheduling to claim submissions.
Infrastructure and interoperability
As with any human, digital workers with the right credentials can access core platforms. Once in these systems, such as EPIC and Cerner, they can quickly connect them without the need to re-enter data.
How Does Healthcare Automation Help Patients and Staff?
Boosting staff satisfaction
With staff turnover at record highs, healthcare organizations are exploring ways to improve the way they work. One place ripe for automation is day-to-day manual tasks, such as data collection and entry. The result is happier staff and more free time to provide care to patients.
Improving patient outcomes
The main goal for healthcare organization is to improve outcomes for their patients. But there’s a growing realization that collaboration and personalization will be the twin trends that drive them. It’s not just treating diseases and conditions, but working with other agencies using automation and analytics to predict and prevent them from happening in the first place.
Enhancing patient experience
Healthcare automation is all about making life easier for already concerned or stressed patients. Self-service portals, remote consultations, digital sign-ins, efficient billing and smart follow-up care plans all improve patient experience and can be enabled by healthcare automation.
Did you know?
When asked what the most important benefit of automation is, most respondents (87%) rated the reduction of manual work, such as re-entering data, as either ‘very’ or ‘extremely’ important.
Source: Blue Prism Global Healthcare Survey
How to Prepare for Healthcare Automation

Once organizations have decided to implement healthcare automation, they build a business case to secure investment. There are a few things to bear in mind before starting on an automation journey, from selecting the right platform to articulating a vision and identifying processes for automation.
Building your Healthcare Automation Business Case
The business case builds a case for committing a budget to a healthcare automation project. As well as outlining the purpose of the project, it helps to clearly articulate the proposition, while allowing assessors to easily compare the different options.
Deciding on your Automation Deployment Method
The business case will lay out the options for hosting the healthcare automation platform, including a public cloud such as AWS, software-as-a-service (SaaS) or an on-premises system. The decision made will depend on the organization’s cloud and digital strategy, as well as the comparative costs of different hosting options.
Selecting the Right Healthcare Automation Partner
It’s important to show which automation platform is being procured and why, how it will be undertaken per procurement rules and regulations and what the long-term licensing costs of the platform will be.
Launching a Successful Healthcare Automation Program
The most successful healthcare automation programs are not just allowed to happen but involve a lot of thought and forward planning. This includes having goals and a vision in place, together with return on investment (ROI) targets based on key performance indicators (KPIs) linked to the organization’s automation strategy.
- Set your goals: what is healthcare automation designed to deliver in terms of process transformation?
- Articulate your vision: where is the organization headed because of healthcare automation, and how will it impact its success?
- Identify processes: how will processes be selected for automation and why, and how will success be measured?
Building a COE Team for Automation
To ensure that healthcare automation activities can effectively scale as demand increases, it’s a good idea to plan where this capability sits within the business. Different models include setting up a center of excellence (COE) that includes relevant staff, such as process analysts and technical architects.
How to Prepare to Launch your First Automation
A good place to start is by launching healthcare automations with a simple but high-volume task, where multiple members of the team typically handle different elements of the process. This showcases success quickly, in a way that is quantifiable and meaningful to the staff who are affected by the change.
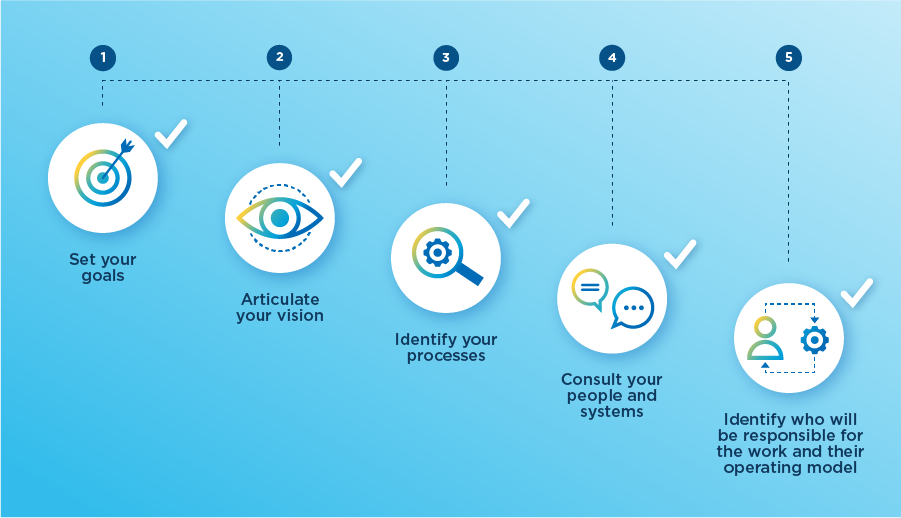
Checklist for Healthcare Automation
1. Set your goals.
2. Articulate your vision.
3. Identify your processes.
4. Consult your people and systems.
5. Identify who will be responsible for the work and their operating model.
Did you know?
The adoption of automated processes in the global healthcare industry has grown steadily over the past five years, from 53% of professionals saying they were moderate or heavy users of automation five years ago to 74% today.
Source: Blue Prism Global Healthcare Survey
Scaling your Healthcare Automation Program
When establishing an intelligent automation program, one of the biggest challenges healthcare providers face is figuring out how to sustain and scale their activities, so they deliver transformative outcomes across the enterprise. With the right planning and strategy, healthcare providers can avoid these problems.
Five Reasons Why RPA Programs Fail to Scale
- Unclear goals and unrealistic expectations
Intelligent automation platforms are very powerful, but expectations must be met with what’s possible. Failing to plan properly early on can be a major obstacle to the success of a healthcare automation program. It’s possible that the first few automations could go well, but without proper goals, planning and expectations (such as KPIs and forecasted ROI), automation can end up going nowhere and never meet scaling expectations. - Lack of understanding about what to automate
A challenge that many healthcare providers face is not knowing which processes to prioritize for automation. This can restrict their ability to scale if there’s a limited pipeline in place or incomplete ideas of what to automate to drive scale and value. - The platform chosen isn’t built for enterprises
Not all automation platforms are the same, and while some might be ideally suited for small, localized automation programs, they may not be suitable for scaling up. - Resistance to change
There can be resistance if change management is not undertaken effectively, or when there has been a lack of communication about shifts that are happening and what it means for day-to-day operations. People tend to be uncomfortable with ambiguity and unexpected change, and process automation will impact different areas of the business. Lack of stakeholder engagement can also have an effect, and many projects fail to scale due to a lack of senior buy-in from the business. Programs can end up siloed in one department or function without senior sponsorship. - Lack of cultural adoption
Preparing an organization for change is often as much about cultural shifts as it is about the technology implemented. In programs that fail to scale, people don’t understand how digital workers can support them with their work — or how they can create an organization that is agile, flexible, and fit for the future.
Did you know?
When asked what the biggest roadblocks are to further digitization, the biggest problem was seen as ‘cultural adoption,’ by 36% of healthcare providers.
Source: Blue Prism Global Healthcare Survey
How Can you Drive the Success of Healthcare Automation?
Now that healthcare providers have successfully implemented intelligent automation for several years, there are many success stories to read about, as well as best practices to consider.
Robotic Operating Model (ROM2)
Blue Prism's ROM2 framework makes it easier than ever to implement automation. It gives you step by step guidance on how to successfully launch, maintain and scale your IA program. Our five ROM2 foundations will help you to build and tailor your automation program so you can expand your IA and create a strategy to transform your organization.
The ROM2’s five foundations are criteria you’ll build to ensure your organization has a robust automation capability:
- Strategy
Developing a strategy and governance framework in line with your organization’s key vision. - Workforce
Transitioning into a unified workforce by seamlessly connecting employees and digital workers. - Design
Discovering opportunities for your organization’s digital transformation by researching, consulting and designing your RPA operating model. - Development
Aligning your IA delivery methods for improved integration. - Operations
Using best practices to reach a streamlined workflow and maintain control of business operations.
Accelerate Automation with a COE
It’s important to keep the development of a COE top of mind when moving from implementation to automation at scale. We’ve seen COEs make a real difference in organizations, whether they’re big or small or oversee a completely centralized or federated operational model.
As automation scales, a standardized approach that ensures an automation strategy doesn’t stray far from overall business goals, gets harder. This is usually because there’s so much going on. Using a COE to take full control and guide the strategy in the right direction makes sense
Maximizing Adoption
Keeping staff onboard with healthcare automation is vital, and we advise organizations to follow these top three tips for maximizing adoption:
- Talk about digital workers as part of the team.
By personalizing new digital colleagues, it’s not only easier to embrace them into the team but to imagine the types of work teams can pass on to them. - Give them names.
Many healthcare providers have accelerated adoption by holding digital worker naming competitions, incentivizing their teams to get behind the process by coming up with the wittiest and best fitting name for their new team members. - Shout about success.
An organization will only know how amazing an automation program is if they hear positive news. Once the word spreads about how much digital workers are giving back to your organization, demand for automation will only spread further.
Automation Lifecycle Management/Governance
Automation at scale can become complex or even chaotic without a well-formed governance structure. A great way to achieve this is by having a centralized place in the COE to manage every stage of the automation lifecycle. This not only gives control through different access levels but also gives a place for the COE and the business to work together on making automation at scale happen.
Keeping a Healthy Automation Pipeline
To truly scale, healthcare providers need to ensure that automation is spread across departments and fully embedded in the fabric of their organizations. The result of this approach is that it becomes ingrained in teams’ thinking and transforms the way they operate. It also helps organizations keep all the information on their processes in one place to simplify success tracking.
Five Healthcare Automation Use Cases

The biggest goal for healthcare providers to achieve from intelligent automation is how to reduce inefficiencies in the delivery of treatments, addressing everything from scheduling patient appointments to sharing patient data across applications, and from reducing waiting times to managing financial applications more efficiently.
Almost everywhere you look in the healthcare sector, there are opportunities to improve manual and reduce repetitive tasks and, most crucially, return time to healthcare professionals to care for their patients.
Below are processes that are good candidates for automation:
- Revenue cycle management
From prior authorization, coding, and remittance to everything in-between, healthcare providers can ensure that they manage their revenue cycle efficiently using intelligent automation. They can enable their teams to deliver efficient patient onboarding, reclaim the cost of care and eliminate confusion around payment responsibility and eligibility with the support of a digital workforce.Learn more about Revenue Cycle Management Automation from our customer Mass General Brigham
- Patient Record updates and data entry
Providing quality healthcare during a pandemic was an acute challenge for the healthcare industry globally, and NHS Aneurin Bevan Health Board in the UK was no exception. Using intelligent process automation, Aneurin Bevan pulled patient information from its PAS and linked it with over one million COVID-19 records to ensure front-line staff in the hospital could immediately see whether an incoming patient had been vaccinated. This has improved patient management, reduced the time needed to triage patients, reduced human errors, and created a safer way to treat them.
Learn more about electronic health record (EHR) automation
Read our blog Healthcare Data Automation - Healthcare supply chain automation
King’s College Hospital NHS Foundation Trust (KFM) is one of the busiest teaching hospitals in London, and it can be difficult to keep it stocked with optimum levels of medical supplies. KFM, responsible for procurement at the Trust, is using digital workers to automatically order supplies that are running low and check incoming invoices. This has enabled the Trust to reduce the time between order and delivery from eight days to just three.
Learn more about healthcare supply chain automation - Invoice Automation
The pharmacy department at King’s College Hospital NHS Foundation Trust in London was dealing with thousands of supplier invoices per year in multiple formats, which needed to be manually matched with orders on the Trust’s core systems. By giving the task over to digital workers, the Trust has fully automated the process, freeing up staff to take on higher-value work.
Learn more about invoice automation in healthcare - Integrated care
The pandemic highlighted why healthcare providers need to work closely with other agencies. Healthcare automation enables them to establish collective strategies, manage shared resources, set the benchmark for best practices, and standardize care — all initiatives that top the priority list for healthcare boards across the world.
Download our ebook on integrated care and healthcare automation
For more examples of healthcare automation, read our RPA use cases in the healthcare blog. To find out about our healthcare automation solutions visit our healthcare RPA page.
Read Intelligent Automation in Healthcare: Examples and Case Studies
Intelligent Automation in Healthcare: Adding AI, ML, and Intelligence
Process Intelligence
There’s no shortage of data in the healthcare sector, from patient health records to monitoring information, and from appointment booking systems to payment schemes. The challenge comes in organizing this wealth of data to create a real-world picture of a hospital or healthcare ecosystem.
With a system like Blue Prism Process Intelligence Powered by ABBYY Timeline, process footprints created in almost any IT application, including EHR, ERP and LIMS, can quickly be extracted, combined and automatically reconstructed in digital form.
This means organizations can visualize processes, such as patient sign-ins, initial evaluation and diagnosis, treatment, medication management, continued care, billing and more. They can identify bottlenecks, often caused by manual inputs, and introduce improvements.
OCR and Document Processing/Decipher IDP
Documents are the common currency between different teams and people and, whether paper or electronic, they come in multiple formats which means the data within them often needs to be re-entered by humans from one system to another. Blue Prism's Document Automation and IDP puts the power of OCR, machine learning(ML), and artificial intelligence(AI) in organizations’ hands to enable greater operational agility.
Whatever your questions may be about healthcare automation and no matter what stage your project has reached, there’s a wealth of advice available, tools to use, and success stories to read. If you have any questions about Blue Prism and how we could support your healthcare automation objectives, please contact an expert.
Read our blog case studies on Intelligent Automation in Healthcare